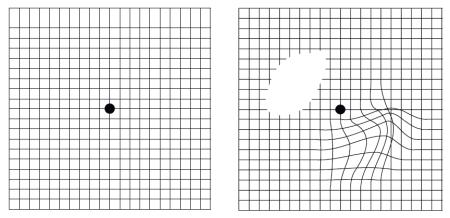
Vision is blurred both at distance and up close. The cornea is thinned and distorted, causing irregular astigmatism and myopia. The image is formed on two different planes.

Keratoconus is classified into four stages, and its progression may ultimately lead to a corneal transplant.
The goal of keratoconus treatment is to regularize astigmatism and correct some of the myopia. When keratoconus is advanced, treatment can also delay the need for a corneal transplant or even eliminate the need for this surgery.
The two gold-standard techniques to date are intracorneal rings and Cross-Linking (CXL).
Indications:
At stage 1, when the cornea is clear with myopia and astigmatism well corrected by glasses or contact lenses (most often soft or rigid), keratoconus can be treated with the Cross-Linking technique.
At stages 2 and 3, when the cornea is still clear but the astigmatism is too severe to be corrected with glasses (only rigid contact lenses allow for effective vision at these stages), keratoconus can be treated by placing intracorneal rings.
At stage 4, when vision can no longer be corrected with rigid lenses and the cornea shows opacities obstructing vision quality, a corneal transplant is necessary.