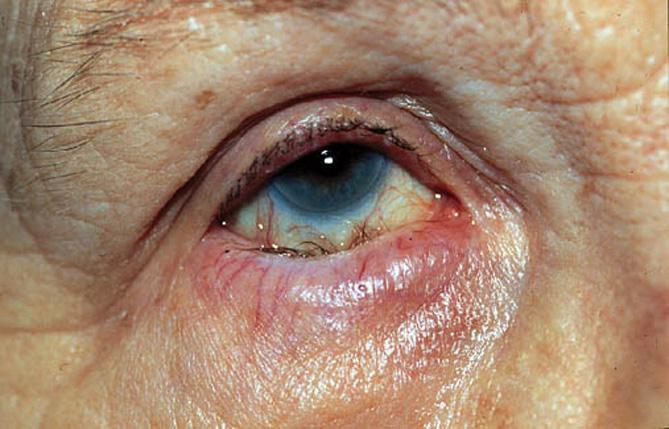
Cataracts correspond to the opacification of the crystalline lens (a normally translucent, high-power lens located inside the eye). Every year, 570,000 people are operated on in France. Surgery is the only way to improve vision altered by cataract.
There are no alternatives to cataract surgery.
Because neither eye drops nor lasers can cure an established cataract. In very advanced cases, cataract can cause blindness.
Worldwide, it is the leading cause of blindness due to the impossibility of large-scale treatment in third world countries. Tens of millions of people are waiting to be operated on, but unfortunately, due to a lack of human and financial resources, many of them will no longer be able to see because of their cataracts. For this reason, many humanitarian trips are organised, particularly to Africa.
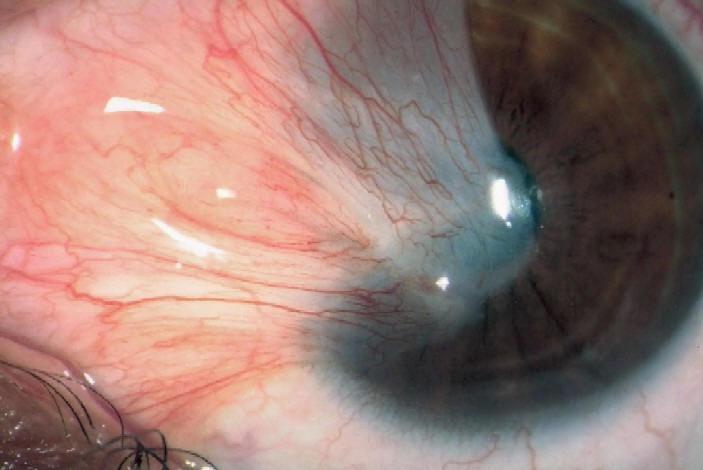
Intervention is defined when the opacification of the lens is sufficiently significant, vision deteriorates slowly, often in distance vision with sometimes paradoxically a transient improvement in near vision without glasses.
The degree of discomfort is not the same for everyone. The decision to undergo an operation is therefore the result of a joint agreement between the ophthalmologist and the patient. Without surgery, the cataract will become denser and vision worse, and this may eventually affect fundus examination. Long-term cataract surgery has a current success rate of over 99.5%.
The surgery:
The procedure is usually performed under local anaesthetic using powerful anaesthetic drops.
Once the eye has been anaesthetised, a micro incision (approximately 2.2 mm) is made at the extreme periphery of the cornea. Then, using a ultrasound probe, the nucleus of the crystalline lens is destructured without damaging the capsule separating it from the posterior part of the eye (this is known as ‘phako-emulsification’). The nucleus of the crystalline lens is then removed to be replaced by a flexible implant. This is inserted folded, then unfolded where the crystalline lens used to be. There are several types of implant.
Currently, the femtosecond laser is used in cataract surgery.
It enables a precise incision to be made, the rhexis, a circular ring around the anterior capsule, to be cut and the nucleus to be cut. The result is greater precision and the use of less ultrasound. Its value is still debated.
In around 1 in 3 cases, a secondary cataract develops, corresponding to an opacification of the posterior capsule (left in deliberately during the operation in order to hold the implant in place). If the patient is bothered by a drop in visual acuity or a sensation of haze, this secondary cataract is treated by laser.
The treatment is carried out in consultation after instillation of drops to dilate the pupil. It is simple, safe, fast (usually less than 10 seconds) and painless.