The consequence of a chalazion is inflammation caused by the blockage of the drainage duct of a Meibomian gland, located inside the upper and/or lower eyelid.
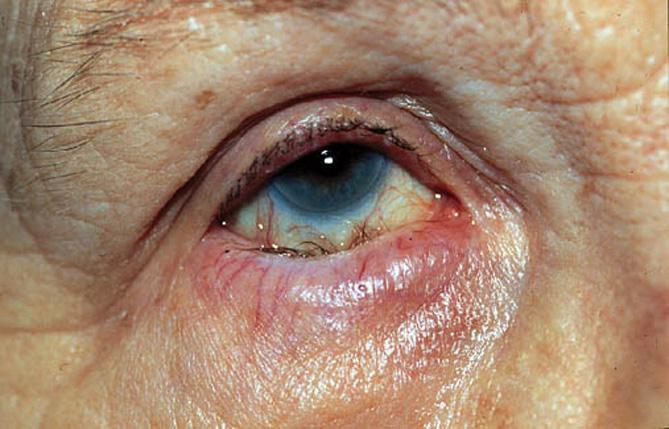
This then manifests as a small bump on the eyelid, which can grow in size and may become red, painful, with a sensation of heat over the course of several days.

Typically, a chalazion disappears after a few weeks, and in this case, there are no medical consequences. A chalazion is not contagious.
Stye and chalazion
Even though a stye is also a bump in the eyelid caused by the obstruction of a sebaceous gland, a chalazion is not a stye. A stye represents an acute infection of the gland. A chalazion is not an infection but rather an inflammation of the area. Inflammation is a process in which the body reacts to a condition and produces swelling, redness, pain, or heat. A stye is usually more painful than a chalazion and may appear infected.
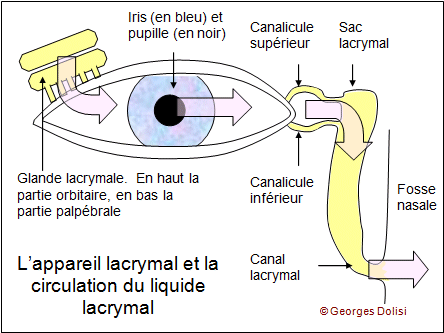
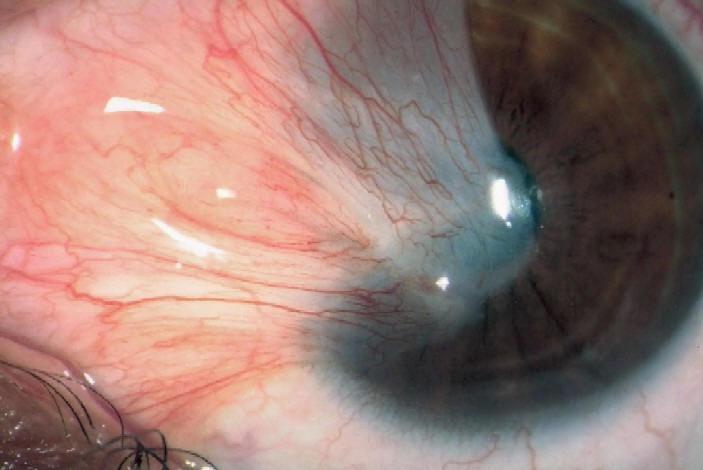
A chalazion is caused by the oil from the Meibomian gland becoming too thick to flow out of the gland. The oil then accumulates within the gland, forming a bump in the eyelid. The gland's wall may rupture, releasing the oil into the tissue of the eyelid, which then causes inflammation of the tissues and sometimes even scarring.
Medical Treatment
The treatment for a chalazion may include the following:
Applying warm compresses for five to ten minutes, four times a day, to reduce swelling and encourage drainage of the gland.
A medical prescription for antibiotic drops or ointments if a bacterial infection is suspected.
Rarely, an injection of a steroid medication into the area of the bump (the chalazion) to help reduce inflammation.
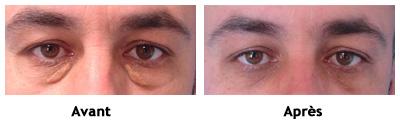
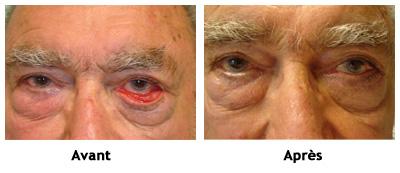
If a chalazion causes significant symptoms or lasts for several weeks, it may be necessary to remove it surgically. If the appearance of the chalazion bothers the patient, surgical removal may also be performed.
In the case of multiple chalazia or recurrent chalazia, the possibility that the patient may have a generalized condition affecting the sebaceous glands should be considered. This is the case with rosacea: this condition can be treated long-term with oral medication to alter the consistency of the oils produced by the glands.